Abstract
Introduction:
Current guidelines recommend anticoagulation with low molecular weight heparin (LMWH) over vitamin K antagonists (VKA) for the treatment of cancer associated thrombosis (CAT). The use of direct oral anticoagulants (DOACs) is gaining more popularity amongst patients and prescribers given the ease of administration and lower cost compared to LMWH. However, there is limited published data comparing LMWH vs DOACs for the treatment of CAT. Here we report patient outcomes from our clinical experience in treating CAT.
Methods:
We evaluated a prospective cohort of patients referred to our centralized CAT clinic at the Cleveland Clinic Taussig Cancer Institute. This clinic provides urgent outpatient consultation for adult cancer patients with clinical concern for VTE. In effort to standardize initial treatment, reduce variation in care, and minimize the need for hospitalization, a care path was created to recommend LMWH as the preferred anticoagulant for treatment of VTE with rivaroxaban as an alternative based on patient preference or cost. We evaluated clinical characteristics, anticoagulation prescription, VTE recurrence rate, and subsequent hospitalization for patients diagnosed with VTE. Continuous variables were analyzed with t-test, chi-square (or Fisher's exact) for unordered categorical data, and Cochran-Armitage test for ordered categorical data. Kruskal Wallis test for age was used when comparing all treatments and Wilcoxon rank sum test for age was used when comparing enoxaparin vs rivaroxaban.
Results:
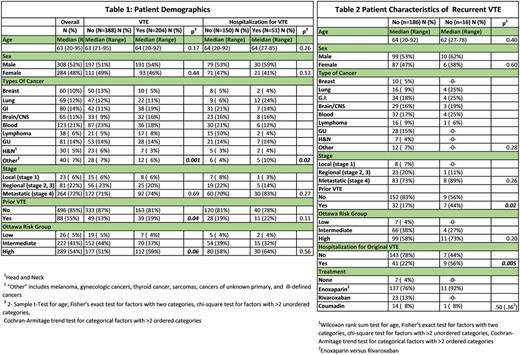
Data from 608 patients seen between 8/2014 and 11/2016 were considered for analysis. Sixteen patients were excluded (15 due to missing data and one because he/she was the only patient treated with apixaban), leaving 592 patients. Males comprised 52% (308/592) of the study population, median age was 63 (range 20-95). Hematologic malignancies comprised 21% (123/586) of patients and most patients with solid tumors had metastatic disease (72%, 265/368). Within the study population, 15% (88/584) had history of prior VTE and 54% (289/537) were considered high risk based on the modified Ottawa score. (Table 1)
VTE was diagnosed in 34% of patients referred to the clinic: Of these, 29% (174/529) were diagnosed with deep vein thrombosis (DVT), 2 % (12/529) with pulmonary embolism (PE), 3% (17/592) with both DVT and PE and one patient had visceral vein thrombosis. Of patients diagnosed with VTE, 25% of patients were subsequently hospitalized.
Gastrointestinal, brain, and lymphoma's had a higher rate of VTE than other tumor types (45-49% vs 29-35%). Breast cancer had a lower rate of VTE than other cancer types (17%, p=0.001)
Enoxaparin was the most commonly prescribed drug given to 76% (149/195) of patients. Rivaroxaban was given to 12% (23/195), 8% (16/195) were treated with Coumadin and 7 patients (4%) were not given anticoagulant therapy due to a contraindication. High Ottawa score patients received rivaroxaban less frequently than other treatments (p=0.02). Patients treated with rivaroxaban had less hospitalizations compared to patients treated with other anticoagulants (p=0.04).
Of patients diagnosed with VTE, 16 (8%) had a recurrent event. There were no significant associations with sex, age, type of cancer, stage, or type of anticoagulant. Specifically, there was no difference in risk of VTE recurrence in patients treated with LMWH (11 events) vs rivaroxaban (0 events); p=0.36). The Ottawa score did not statistically correlate with recurrent VTE (0%, 6%, and 10%) for low, intermediate, and high risk, respectively (p=0.2). An increased risk of recurrent VTE was seen in patients who had personal history of VTE and in those who were hospitalized after the VTE (p=0.02 and p=0.005, respectively). Table 2
Conclusion:
The Cleveland Clinic provides centralized care to cancer patients diagnosed with VTE. Among patients referred to our CAT clinic, we found risk of VTE correlates with cancer type and personal history of VTE. Most of our patients received our recommended therapy, enoxaparin, but rivaroxaban was prescribed to some due to patient preference. Patients treated with rivaroxaban had fewer adverse outcomes compared to those treated with other anticoagulants. Limitations include the small sample size and greater use of rivaroxaban in lower risk patients. We found the risk of VTE recurrence was higher in those with history of VTE and in those hospitalized for their VTE event.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal